Diabetes mellitus is a pathological condition characterized by a violation of metabolic processes (metabolism). As in type 1 diabetes, it occurs due to insufficient production of its own hormone, insulin, or a violation of its effect on cells and tissues of the body (type 2 pathology).
The article discusses in detail the main types of diabetes mellitus, their causes and differences in the mechanisms of development, as well as a description of the characteristics of the treatment of patients.
A little about insulin and its role in the human body
Insulin is a hormone produced by the pancreas. The organ is located behind the stomach, surrounded by the spleen and a loop of the duodenum. The weight of the pancreas is about 80 grams.
In addition to hormones, the gland produces pancreatic juice, which is necessary for the digestion of lipids, carbohydrates and proteins. Insulin hormone is synthesized by β-cells. They are localized in small groups called islets of Langerhans on almost the entire surface of the pancreas. The islets also contain α-cells that synthesize the hormone glucagon. This hormone has the opposite effect on insulin.
Insulin is a protein molecule consisting of several amino acid chains. Its task is to absorb glucose (sugar) by the cells of the body. Sugar is necessary for a person to get energy. Without it, cells and tissues cannot cope with their functions.
In parallel with sugar intake, insulin also regulates the entry of amino acids into cells. Amino acids are considered one of the main building materials. Another function of insulin is the accumulation of lipids in the body.
Classification of diabetes
According to the classification of diabetes generally accepted and used in modern endocrinology, the pathology is divided into the following types:
- Type 1 - insulin dependent (IDDM);
- type 2 - non-insulin dependent (NIDDM);
- form of pregnancy;
- specific types of diabetes.
The last option is a group of pathological conditions that differ from each other in their pathogenesis and developmental reasons. These include genetic defects in the insulin hormone or insulin-secreting cells, diseases caused by the effects of chemicals and drugs, diabetes due to infectious processes, etc.
All types of diabetes are associated with hyperglycemia. This is a condition that manifests itself with an increase in the level of glucose in the blood. Confirmation or denial of the diagnosis of diabetes is based on the diagnosis of glycemia numbers.
1 type
Type 1 pathology (ICD-10 code - E10) is considered an autoimmune process resulting in the death of insulin-secreting cells. Simply put, such processes begin in the human body, when its own immune cells consider pancreatic cells to be foreign and destroy them.
As a rule, the insulin-dependent type is caused by a hereditary tendency, but at the same time provocative factors also play an important role. Statistics show that the presence of pathology in a child is possible in the following cases:
- if the mother is sick - with a frequency of 2%;
- sick father - 5%;
- sick brother or sister - 6%.

The autoimmune process, that is, the presence of antibodies against the pancreas' own cells in the body, occurs in more than 80% of insulin-dependent patients. Often, in addition to type 1 disease, diabetics suffer from other autoimmune diseases, such as chronic adrenal insufficiency, pancreatic diseases, vitiligo, rheumatism.
How does it develop?
Typically, clinical signs of the disease appear when more than 85% of insulin-secreting cells have already died, but depending on the individual characteristics of the body, this period may vary during its duration. It often occurs during childhood and adolescence. It happens that young patients learn about the existence of the disease already in the period of acute complications, for example, in a ketoacidotic state.
Lack of energy and lack of insulin leads to the massive breakdown of fats and proteins, which explains the patient's weight loss. High blood sugar causes hyperosmolarity, which is manifested by massive urine production and the development of signs of dehydration. Since there is not enough insulin, the body suffers from energy starvation, as a result of which there is an excessive synthesis of counterinsular hormones, that is, hormones that have the opposite effect on the work of insulin.
These hormones include cortisol, glucagon, and somatotropin. They stimulate the production of glucose in the body, despite the fact that the level of sugar in the blood has already crossed the roof.
The massive breakdown of fats leads to an increase in the number of free fatty acids in the blood. This is a trigger for the formation and accumulation of ketone (acetone) bodies, which become provocateurs of the ketoacidotic state. If such a pathology continues to progress, the patient may fall into a coma or even die if dehydration and the pH of the blood shift to the acidic side.
Symptoms
Type 1 diabetes is characterized by the development of bright symptoms that increase in severity over several weeks. Diabetic patients complain:
- for the formation of a large amount of urine;
- excessive thirst;
- constant itching of the skin;
- lose weight.
Weight loss accompanied by normal or increased appetite is one of the symptoms that distinguish type 1 pathology from other types of diabetes mellitus. The patient is worried about acute weakness, he cannot do his usual work, he feels sleepy.
The progression of the clinical picture is accompanied by the appearance of the smell of acetone in the exhaled air, abdominal pain, nausea and vomiting, severe dehydration. If the disease appears at a later age (about 40 years), the symptoms are not so obvious and, as a rule, the presence of the disease is determined during a clinical examination.
type 2
Non-insulin-dependent diabetes mellitus (ICD-10 code - E11) is a chronic pathology in which high blood sugar levels occur due to insulin resistance. Later, the function of the β-cells of the islets of Langerhans is also disturbed. In parallel with carbohydrate metabolism, pathology also affects the process of fat metabolism.
Hereditary predisposition is one of the main causes of type 2 diabetes. If one of the parents has a disease, children get sick in 40% of cases. But heredity alone is not enough, provocative factors:
- high body weight;
- low physical activity;
- increased blood pressure numbers;
- high level of triglycerides in the blood;
- having a baby born weighing more than 4 kg in the past;
- having gestational diabetes in the past;
- polycystic ovaries.
Currently, the number of patients with type 2 diabetes is increasing. This form of pathology accounts for more than 85% of all clinical cases. Middle-aged and older men and women are more likely to get sick.
How does it develop?
The mechanism of development is based on the emergence of insulin resistance, that is, the pancreas produces enough hormones to transport sugar molecules to the cells, but the cells themselves lose sensitivity to this substance. The result is hyperglycemia.
In order to reduce the blood sugar level, the gland begins to work to the limit of its capabilities. This leads to the depletion of insulin-secreting cells.
The appearance of ketoacidosis is not typical for the second type of pathological condition, because even a small part of the hormone is synthesized by the islets of Langerhans.
Symptoms
The disease usually manifests itself in patients over 40 years of age. In most cases, the clinical picture is combined with the appearance of pathological body weight, changes in fat metabolism in blood tests. Associated symptoms:
- performance is slightly reduced, but it is not as obvious as in the first type of the disease;
- pathological thirst;
- excessive urination;
- women may be bothered by itching of the skin in the genital area and perineum;
- rashes appear on the skin that do not heal for a long time;
- discomfort, numbness in the lower extremities and a feeling of vomiting.
Type of pregnancy
The WHO classification of diabetes includes the gestational form of the disease (ICD-10 code - O24). It is typical for pregnant women. 5-7% of patients who give birth to a baby suffer from diabetes. The WHO classification of diabetes and its types includes another name for this type of pathology - diabetes in pregnant women.
If the disease appeared in a woman before the moment of conception of the child, it is considered during pregnancy, during pregnancy - pregnancy. Currently, the mechanism and causes of the disease are not fully understood. There is information about the role of genetic predisposition. Risk factors can be:
- physical and mental trauma;
- infectious diseases;
- pancreatic diseases;
- including a large amount of carbohydrate-rich foods in the menu.
The gestational form can manifest itself as a manifestation, that is, a bright clinical picture or a violation of glucose tolerance. Pathology, as a rule, disappears on its own after the birth of the baby.
A woman becomes a member of the group of patients with a high risk of developing non-insulin-dependent diabetes mellitus in the next 10-15 years.
During the birth of a child, a woman's body undergoes certain changes related to the hormonal field. This is due to the functioning of the placenta, which secretes the following hormones:
- chorionic gonadotropin;
- progesterone;
- estrogens;
- corticosteroids, etc.
All these hormonally active substances lead to the appearance of insulin resistance. At this stage, hyperplasia of insulin-secreting cells from the pancreas and the release of a large amount of insulin into the blood are observed. The appearance of insulin resistance leads to the fact that the woman's body begins to actively use the metabolic products of fats, and sugar is stored for the nutrition of the fetus. The disease develops in the conditions of the combination of the hereditary tendency to diabetes and the above-mentioned factors.
Symptoms
The gestational type of the disease manifests itself in the same way as other types of diabetes, but the symptoms are slightly less pronounced. A woman may not pay attention to the symptoms, associating its occurrence with her "interesting" position. If the clinical picture is revealed, a pregnant woman can make the following complaints to the attending physician:
- dry mouth;
- constant desire to drink;
- excessive urination;
- increased appetite;
- reduced performance and vulnerability;
- itching and burning in the genital area.
It is important! Usually the disease develops at the end of the second or the beginning of the third trimester.
Effect of pathology on mother and fetus
Chronic hyperglycemia has a negative effect on both the mother's body and the child. Pregnancy can be complicated by:
- polyhydramnios;
- late gestosis;
- termination of pregnancy at different stages of pregnancy;
- the birth of a child with a large body weight (more than 4-4. 5 kg).
Babies born to sick mothers have a characteristic appearance. The shoulders are wide enough, the subcutaneous fat is pronounced, the face has a round moon shape. There is significant swelling of the skin and hypertrichosis. The most serious complications of the disease are the death of the fetus during the development of the fetus and the death of the newborn baby. As a rule, such conditions occur in the presence of a pregestational form of the disease.

Special species
We are talking about secondary forms of the pathological condition that develop under the influence of chemicals, drugs, infectious processes and other diseases of the endocrine and extraendocrine sphere.
Diabetes can be caused by the following diseases and conditions of the pancreas:
- organ inflammation;
- mechanical damage;
- gland removal;
- neoplasms;
- cystic fibrosis;
- pigmentary cirrhosis, etc.
From chemicals and drugs, nicotinic acid, adrenal cortex hormones, interferons, thyroid hormones and diuretics can contribute to the development of the disease. The list goes on with opiates, rodenticides, antidepressants, drugs used for antiretroviral therapy.
Features of treatment
The treatment of the pathological condition is selected individually for each clinical condition. The treatment scheme and methods used depend on the degree and type of diabetes, the brightness of the clinical picture and the presence of complications. A qualified endocrinologist will tell you how to determine and confirm the presence of the disease. He will prescribe the following diagnostic methods:
- general blood and urine tests;
- capillary blood analysis for glucose from a finger on an empty stomach;
- blood biochemistry;
- urine analysis for sugar;
- glucose tolerance test - mandatory for all future mothers in the period from 22 to 26 weeks of pregnancy;
- determination of indicators of glycosylated hemoglobin.
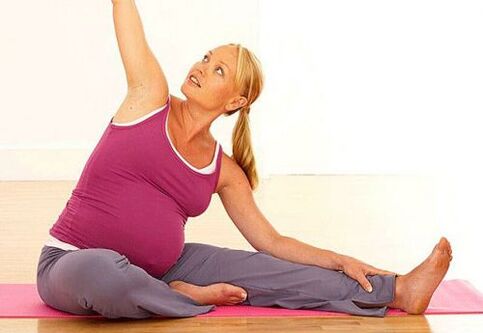
Therapeutic measures include not only taking drugs, but also physiotherapy exercises, correction of nutrition, teaching the patient self-control.

self control
Diabetic patients should record their feelings, glycemia, sugar level in urine, and also record information about individual menus and physical activity during the day. The totality of such indicators and their accounting is self-control. The purpose of such measures is not only to control the level of sugar, but also to interpret the results, as well as to plan one's actions when the numbers are outside the acceptable range.
With normal health, it is important to measure the sugar level at home and record these indicators at least once a day. Any change in well-being requires clarification of the amount of glucose in the blood several times a day:
- before each main meal;
- some time after food enters the body;
- before evening rest;
- in some cases, morning measurements on an empty stomach may be required.
Urine glucose is also measured at home. This requires the availability of express lanes. They can be bought in pharmacies. The presence of sugar in the urine will indicate that the level of glucose in the blood is more than 10 mmol / l, because this number is the renal threshold at which glucose molecules penetrate into the urine.
If the patient travels, is actively involved in sports or has any additional diseases, more strict self-monitoring will be required.
In order for a person with diabetes to live comfortably on a daily basis, it is necessary to purchase the following personal devices and devices:
- glucometer with lancets, test strips and necessary accessories;
- express urine strips that measure the level of acetone bodies and sugar;
- tonometers to clarify blood pressure figures;
- a self-monitoring diary in which all the necessary information will be recorded.
Food
Correction of individual nutrition is the basis for the treatment of all types of diabetes. Changing the personal menu with type 1 allows you to reduce the load on the pancreas, reduce the amount of carbohydrates given to the body. A low-calorie diet in type 2 diabetes can not only achieve the above goals, but also reduce pathological body weight.

Patients should strictly monitor their daily calorie intake. For each patient, his weight, age, gender, energy consumption, physical activity, and drug treatment used are calculated individually. It is necessary to limit the intake of carbohydrates and high-calorie foods in the diet of patients. Proteins are not only possible, but also necessary, fats should be slightly limited, especially with type 2 pathology.
Patients should understand the system of bread units, glycemic and insulin indices of products, calories. Features of nutrition principles:
- do not eat more than 8 bread units in one meal;
- sweet liquids (lemonade, sugary tea, store water) are prohibited;
- sweeteners are used instead of sugar, homemade compotes and fruit drinks are used instead of store-bought juices;
- the number of bread units must be planned in advance, because insulin is given before the products enter the body;
- food should be in small portions, but often;
- patients should drink enough fluids - restrictions may be present in case of renal failure or other complications accompanied by edema.
You can read more about prohibited foods, as well as those that should be consumed without fear, in the table.
|
|
|
The possibility of alcoholic beverages is discussed individually. If there is compensation for diabetes, if there are no complications, if the patient feels normal, a small amount is allowed. Beer and sweet cocktails are prohibited.
Treatment
Treatment of IDDM and gestational form is based on insulin therapy. This is the process of administering hormonal preparations based on insulin to replace the lack of its own substance in the body. There are several groups of drugs that differ in the duration of action and the speed of onset of action: ultrashort drugs, short, medium-term hormones and long-term insulins.
Usually, doctors combine two drugs with different duration of action at the same time. This is necessary to create the most physiological conditions for the pancreas.

Type 2 disease requires the use of hypoglycemic tablets. The main groups are biguanides, sulfonylureas, thiazolidinediones, glinides, etc.
Differential diagnosis between types of diabetes mellitus should be performed only by a qualified specialist. He will also help to choose the therapy regimen, the optimal lifestyle and give recommendations that allow the patient to get compensation as soon as possible.
























